A blow to the head is the usual cause of bleeding into or around the meninges, which forms a hematoma. Damage to an artery from a skull fracture, usually on the side of the head, may be the cause of an epidural hematoma (Fig. 1), which appears between the dura mater and the skull bone. The rapidly accumulating blood puts pressure on local vessels and interrupts blood flow to the brain. There may be headache, loss of consciousness, or hemiparesis (partial paralysis) on the side opposite the blow. Diagnosis is made by CT scan or magnetic resonance imaging (MRI). If pressure is not relieved within one or two days, death results.
A subdural hematoma (see Fig. 1) often results from a blow to the front or back of the head, as when the moving head hits a stationary object. The force of the blow separates the dura from the membrane below, the arachnoid. Blood from a damaged vessel, usually a vein, slowly enters this space. The gradual accumulation of blood puts pressure on the brain, causing headache, weakness, and dementia. If there is continued bleeding, death results. Figure 1 also shows a site of bleeding into the brain tissue itself, forming an intracerebral hematoma.
A cerebral concussion results from a blow to the head or from a fall. It may be followed by headache, dizziness, vomiting, loss of consciousness, and even paralysis, among other symptoms. Damage that occurs on the side of the brain opposite the blow as the brain is thrown against the skull is described as a contrecoup (kontre-KU) injury (from French, meaning "counterblow").
Other injuries may damage the brain directly. Injury to the base of the brain may involve vital centers in the medulla and interfere with respiration and cardiac function.
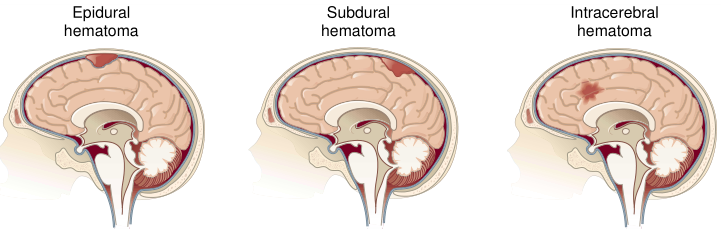
FIGURE 1. Location of epidural, subdural, and intracerebral hematomas.
责任编辑:admin
上一篇:医学文章阅读——Degenerative Diseases
下一篇:Explaining the Tissnes and Structure of the Human Body

微信公众号搜索“译员”关注我们,每天为您推送翻译理论和技巧,外语学习及翻译招聘信息。